Most healthcare, pharmaceutical and clinical research organizations are sitting on a goldmine of data that would substantially improve patient outcomes, if it could be made simpler to access and analyze. Fortunately, new data integration tools can help make personalized medicine a reality — revolutionizing the treatment of cancer and other notoriously complex diseases.
Better data integration also can streamline drug development, medical research and healthcare operations. It can help healthcare and pharma professionals utilize the deluge of new kinds of patient data from genomics, wearable devices, social media and other emerging sources. Ultimately, this can expand treatment options, reduce costs and yield a better overall healthcare experience.
“Imagine a physician has a cancer patient who is not responding to treatment. The doctor might want to know, quickly, whether that patient might be a good candidate for a clinical trial of a new drug,” explained Enkashi Singh, Senior Product Specialist for SAP Health. “Today, that doctor would have to call the hospital’s clinical trial study nurse, who’d manually consult a list of trials that the hospital happens to know about, and try to find some good matches.”
“Now, instead, imagine that the doctor could turn to one system to enter all of that patient’s data and symptoms. Instantly, they’d get a list of relevant clinical trials happening around the world, not just at that one hospital,” Singh continued. “Or, the doctor could quickly define a cohort of similar patients, from anywhere, and analyze information about their treatments and outcomes. That would be a powerful tool to support healthcare decisions. And it all hinges upon effective, smart data integration”

Pharmaceutical companies face especially high stakes regarding data integration. Drug development represents their greatest cost, and it also requires intense attention to risk management.
The obstacle is that too much important data about patients and treatments is locked up in separate silos at different organizations, or even internally within one organization. This might include patient records from a specific healthcare provider, notes from doctors and nurses, pharmacy records, insurance and billing data, research from “fallen angel” drugs, published clinical trials and more. Bridging these silos entails further challenges related to patient privacy, business processes, intellectual property and data standards.
Legacy electronic health record (EHR) systems also represent a considerable challenge to data integration. In general, EHR systems were built primarily to support fee-for-service billing, not to track outcomes. The major EHR vendors are working to transform their systems to support value-based healthcare, but their progress has been gradual. A potentially faster and more robust option is to add a third-party data integration service, which is layered atop an existing EHR and able to integrate data from a variety of other sources.
Once an organization begins to tap its own data silos, integrate the data and share it (even just internally), broader and more useful analyses become possible. The key is to deploy a technology platform and data warehouse which:
- Accommodates many data types and sources
- Supports speedy analysis
- Connects many administrative processes
- Can process unstructured text
Integrating data from many sources helps detect and treat disease
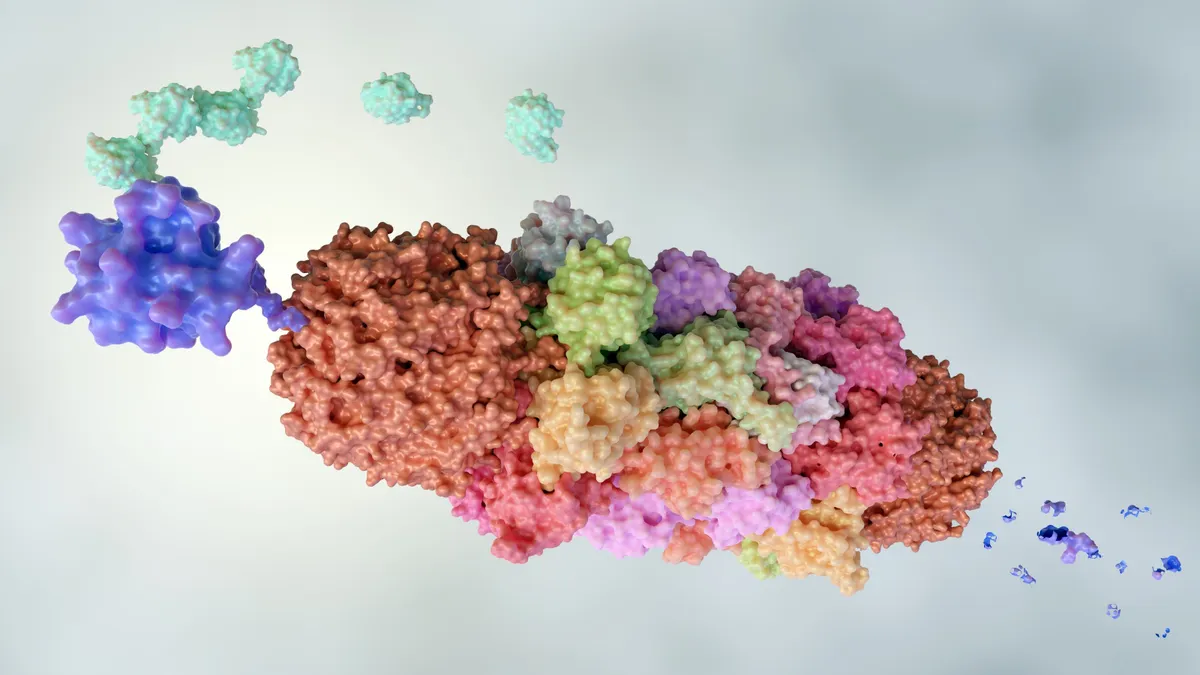
23andMe, a company that helps consumers acquire, understand and use their own genomic data, has expanded its business model by selling anonymized consumer genomic data to the biopharma industry. In September 2017, 23andMe announced that their data had helped Genentech to nearly double the number of known genetic variants associates with Parkinson’s disease.
Meanwhile, CancerLinQ LLC, a wholly-owned nonprofit subsidiary of the American Society of Clinical Oncology (ASCO), partnered with SAP Health to develop CancerLinQ®, a platform that powerfully connects and analyzes real-world cancer care data from electronic health records to improve the quality and value of care for all. More than 100 oncology practices have agreed to participate, and demand among ASCO members has been tremendous.
Also, artificial intelligence is playing a larger role in enabling integrated data to augment the expertise of doctors and researchers. At a 2017 conference, Stanford dermatologist Justin Ko explained how machine learning algorithms, trained on a database of 130,000 images of skin conditions, generally outperformed dermatologists in deciding whether a particular image warranted a biopsy.
Ko experienced this personally in his clinic: “I was on the fence about a mole on my patient’s shoulder. I didn’t see any troublesome features, but my gut didn’t sit well with my gut. So, I pulled out my iPhone, took photos, and fed it to the system,” said Ko. “The result was adamant: this was a malignant lesion. That pushed me to biopsy — and indeed, it turned out to be an early, subtle, evolving melanoma. We caught it at a very early stage, treated it surgically, and that patient will suffer no consequences.”
According to Singh, such diagnostic tools could have profound effects, with help from effective data integration and warehousing. “Think of the impact to a poor rural hospital, or in the developing world,” she said. “They may not have access to advanced imaging tools or expert diagnosticians. But people could snap a picture with a smartphone, or collect data with an app, and get a pretty reliable diagnosis or treatment recommendation.”
Strengthening integration with data standards
An open data exchange standard is essential as the healthcare industry slowly progresses toward a more collaborative, interoperable ecosystem. The Fast Healthcare Interoperability Resources (FHIR) specification is likely to help overcome the tunnel-vision built into legacy proprietary electronic health record (EHR) systems — most of which were initially designed to support fee-for-service billing, not patient outcomes.
Such a standard would make it easier for solution providers with broad data integration expertise to complement legacy EHR systems, by providing a rich, standards-based data integration layer. It also could help pharmaceutical companies and healthcare providers glean valuable insights from huge volumes of data from genomics, wearable devices and social media — data types that EHR systems were never designed to handle.
As data integration proliferates in health-related fields, both existing and new data will yield greater value and better outcomes. New systems will be able to analyze genetic and clinical data on the fly, and re-analyze existing data. As researchers develop new drugs, learn more about disease pathways, or spot new drug interactions, old data will undoubtedly have compelling new stories to tell.