Dive Brief:
- Use of telehealth services among seniors covered by Medicare skyrocketed in the early weeks of the COVID-19 pandemic, when the Trump administration eased regulation of virtual care.
- Almost 1.3 million members received telehealth services in the week ending April 18, compared to just 11,000 in the week ending March 7, according to Medicare claims data.
- Looser regulations will remain in place for only as long as the national public health emergency lasts, but various groups are now calling on the Department of Health and Human Services to permanently relax barriers. Top administration health officials have said they're exploring the possibility.
Dive Insight:
Federal agencies, public payers and large commercial insurers have sought to expand access to telehealth during the pandemic, cutting cost-sharing, removing administrative hurdles and distributing funding to build up communities' digital capabilities.
Seniors are at particular risk for severe illness and complications from infection by the new coronavirus, which has killed more than 105,000 people in the U.S. as of June 3. Telehealth could therefore be particularly important for older Americans, enabling them to avoid coming into contact with potentially exposed individuals at a doctor's office.
There have been some early signs of increasing telehealth adoption, but the Medicare claims data are some of the first data showing just how quickly seniors covered under the program took to virtual care.

"It's not that this was necessarily unexpected, but this is really five to 10 years of progress taking place in a month and a half," Tim Epple, a principal at health consultancy Avalere, told Healthcare Dive.
Previously, telehealth use in Medicare was severely restricted to specific locations and circumstances, like for beneficiaries in rural areas or patients already in a hospital. According to CMS, only 90,000 fee-for-service Medicare members used virtual care through the entire 2016 calendar year — a fraction of the number that used telehealth during the week ending April 4.
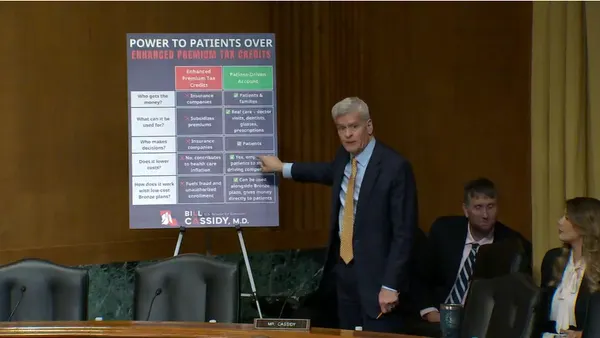
The Trump administration began easing barriers to virtual care in early March, allowing Medicare to temporarily reimburse telehealth appointments at the same rate as in-office visits, and saying it would not enforce HIPAA privacy law penalties curtailing telehealth use. CMS has sharply expanded the number of services available via virtual care, upped payments for audio-only visits and granted a blanket waiver enabling providers licensed in one state to provide services to patients in another.
CMS Administrator Seema Verma told reporters on a May 26 call her department is evaluating the telehealth waivers to determine if they should be extended past the scope of the national emergency. CMS is in the process of additional rulemaking around the issue, she said.
"You'll see that some of the provisions that we have extended on a temporary basis will be made permanent," Verma said.
Health IT and provider groups, along with some politicians, have called on CMS to keep most, if not all, of the changes.
There are some indications telehealth use is flattening after the early explosion in demand, as states begin to slowly reopen businesses, and doctors resume more in-person operations. Outpatient visits have begun to rebound nationwide, according to a report from The Commonwealth Fund, and there are some procedures and treatments doctors can't do digitally.
But analysts say virtual care is likely to remain popular for low-acuity care, like chronic disease management, behavioral healthcare and evaluation visits that can easily be conducted through telehealth, especially if CMS retains telehealth payment parity for Medicare's 44 million beneficiaries.
"There's a huge impetus for those types of services to expand if those recent flexibilities stick," Chad Brooker, an associate principal at Avalere, told Healthcare Dive. "I think that's the biggest question — what remains."