The U.S. government will not give Bluebird bio a green light to offer fertility support to federally insured people undergoing treatment with the biotechnology company’s gene therapy Zynteglo.
In a “negative opinion” issued Monday, the Department of Health and Human Services’ inspector general indicated that Bluebird’s proposed support, which would provide up to $22,500 to cover fertility preservation treatment, could potentially run afoul of anti-kickback payment rules.
The written opinion is advisory. The inspector general hasn’t determined Bluebird’s program actually violates those rules, indicating instead that the government won’t provide the company with prospective immunity against legal action.
Still, it’s a blow to Bluebird’s efforts to broaden use of Zynteglo, which is approved in the U.S. for the inherited blood condition beta thalassemia. While Zynteglo offers dramatic benefits, it also requires preparatory treatment with a chemotherapy that carries a high risk of infertility. Bluebird’s proposed support is meant to aid patients who would otherwise forgo treatment because of that concern.
The rules flagged by the inspector general apply to patients covered by federal insurance programs like Medicaid, not to those covered by commercial insurance.
“No patient should have to choose between a potentially lifechanging or lifesaving therapy and the chance to have a child,” Bluebird said in a statement to BioPharma Dive. “Now, without clear guidance or safe harbor for manufacturers, HHS risks exacerbating an already gaping inequity between patients insured through Medicaid and those who are covered by commercial insurance.”
Bluebird also sought permission to extend the program to people with a neurological disease known as cerebral adrenoleukodystrophy who are being treated with another of the company’s gene therapies, Skysona.
In its opinion, the HHS inspector general cited a lack of sufficient data on costs and access to healthcare services to determine that Bluebird’s plans present a “low risk” of fraud and abuse under anti-kickback rules.
“We recognize that cell and gene therapies consist of an evolving field that holds significant promise for improving the health of patients, including Federal health care program enrollees,” the inspector general wrote. “These treatments are novel, and much is yet unknown about them and optimal arrangements for ensuring appropriate access to them.”
The negative opinion comes one week after Vertex Pharmaceuticals sued the federal government over the inspector general’s block of its plans to provide similar fertility support to people receiving its gene therapy Casgevy. Patients getting Casgevy, which is approved for sickle cell disease and beta thalassemia, undergo the same chemotherapy “preconditioning” regimen.
One possible avenue for collecting more data is a pilot program being put in place by the Centers for Medicare and Medicaid Services, which aims to test different payment schemes for gene therapies for sickle cell like Casgevy. Bluebird’s sickle cell treatment Lyfgenia, which is similarly designed as Zynteglo and was approved alongside Casgevy last December, is also included. The pilot requires manufacturers provided limited fertility support.
Both Bluebird and Vertex have described that requirement as inconsistent with the inspector general’s determinations on their fertility support programs.
“We are also surprised that OIG does not view infertility as a barrier to treatment — particularly since HHS’s own Center for Medicare and Medicaid Innovation clearly recognizes the essential role of fertility preservation through its focus on these services within the Cell and Gene Therapy Access Model,” Bluebird said in its statement.
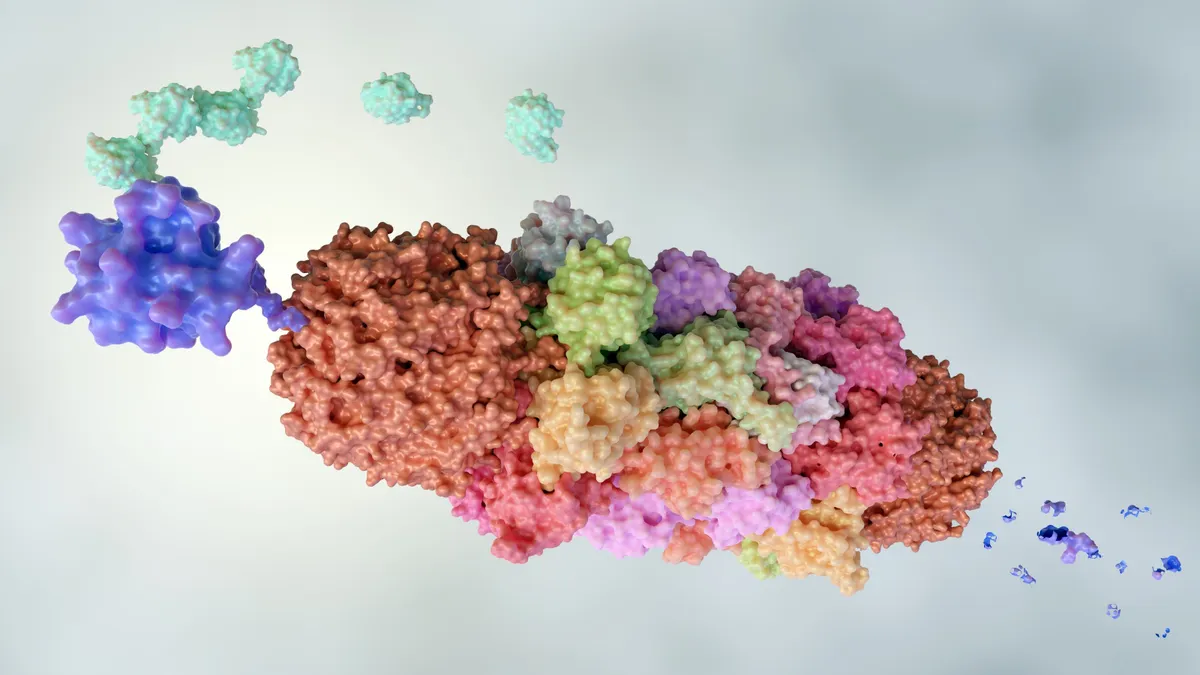
Zynteglo, Casgevy and Lyfgenia are all built from a patient’s own stem cells and then, using various techniques, genetically modified to induce a certain effect once reinfused into the body. The chemotherapy is used to clear out space in the bone marrow for the engineered stem cells to engraft and then mature into functional blood cells.