For decades now, scientists have been experimenting with a new way to target and destroy proteins linked to disease. Unlike most approved drugs, which work by turning cell signaling up or down like a dimmer switch, this approach aims to rid cells of problem proteins entirely.
Targeted protein degradation, as it’s broadly known, could open the door to attacking proteins that remain frustratingly out of reach of traditional drugmaking technology. It may also be a more efficient way to shut down known disease targets.
Earlier this year, the field got its best look yet at how well one common type of these drugs performs. Biotechnology company Arvinas said a medicine it advanced with Pfizer succeeded in a large breast cancer study. The finding marked the first time this kind of drug had made it through Phase 3 clinical testing.
Arvinas and Pfizer were met with more skepticism than praise, however. Their drug, called vepdegestrant, proved only modestly beneficial for some patients and no more helpful for others than an existing mainstay. It doesn’t appear clearly better than other medicines, either, leaving its potential uncertain.
Still, there is growing momentum in the degrader field. Since Arvinas’ findings, another company, Kymera Therapeutics, showed that a protein-destroying medicine it developed may be able to stifle a drug target others have struggled to reach. Multiple deals have been struck by large companies such as Roche and Novartis, suggesting pharmaceutical firms believe degraders have only begun to show their promise.
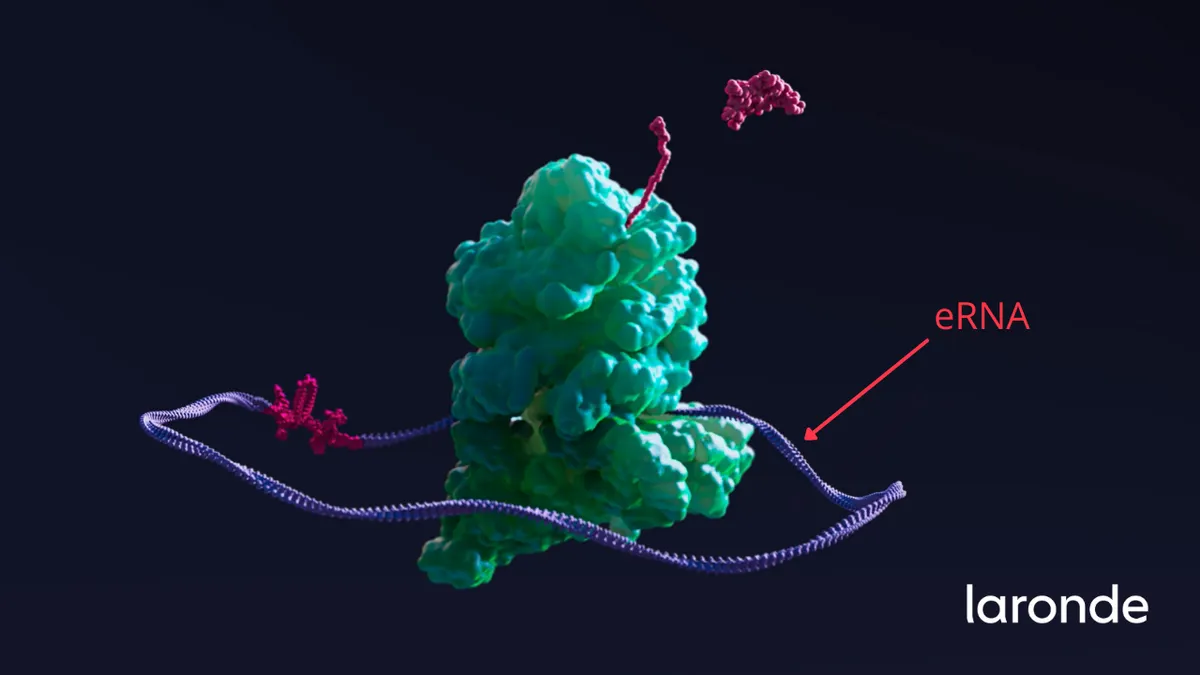
As a drugmaking science, targeted protein degradation has matured since 2001, when scientists Craig Crews, Ray Deshaies and others published a foundational paper on one type of protein-degrading molecule, dubbed proteolysis-targeting chimera, or PROTAC. Since then, more than two dozen biotechs have launched in the field, developing new ways to junk troublesome proteins that carry arcane names like LYTACs, DUBTACs and molecular glues. Several have drugs in or near clinical testing.
“The next five years will see many degraders approved with potential huge impact for patients,” predicted Nello Mainolfi, CEO of Kymera.
“Drug discovery is a risky and costly endeavor,” said Angela Cacace, Arvinas’ chief scientific officer. “Our modality has the potential to transform the way we treat diseases, including horrible, lethal diseases like cancer and neurodegeneration.”
What is targeted protein degradation, and how does it work?
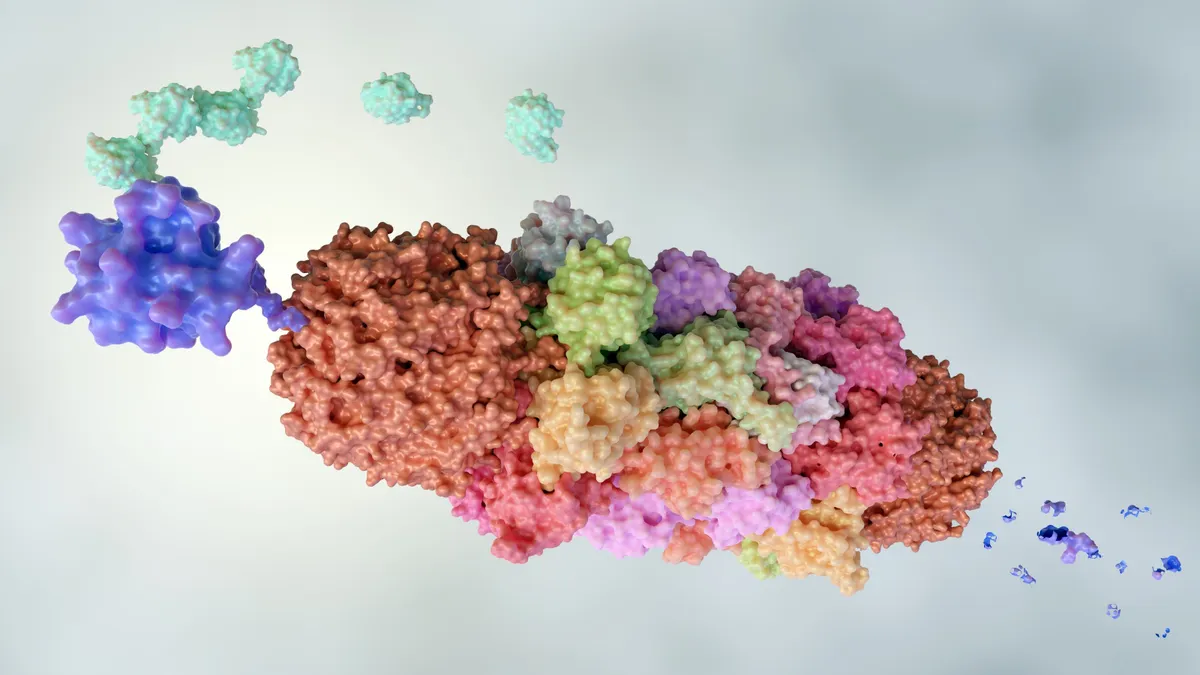
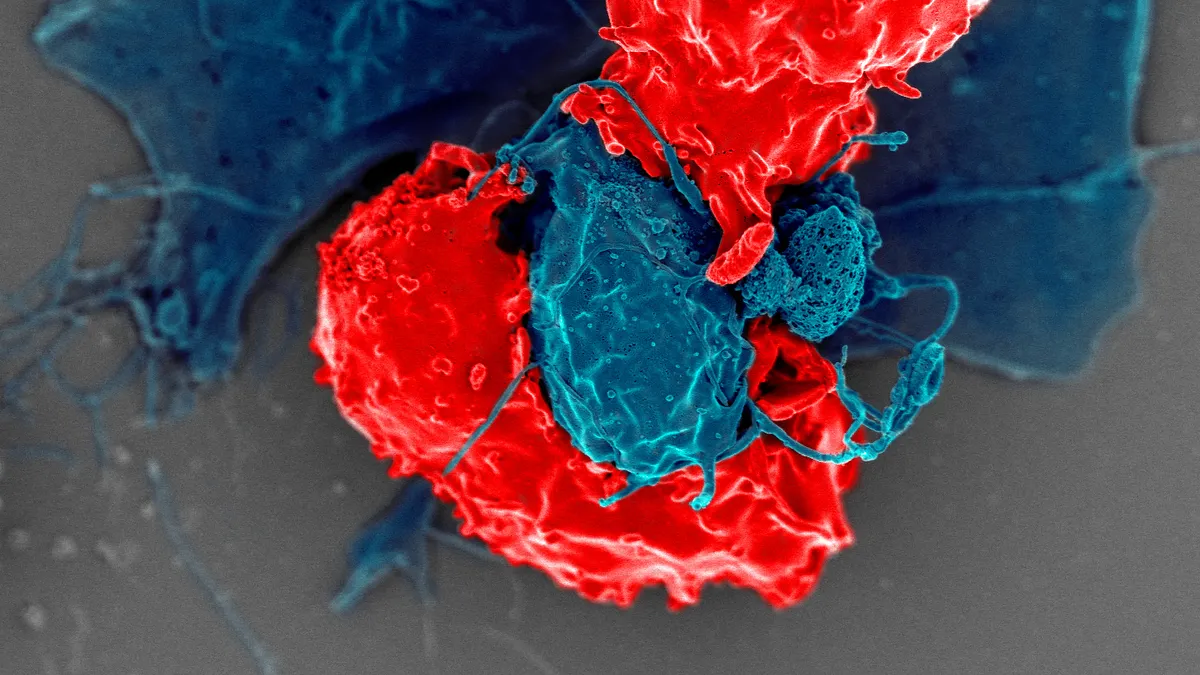
The body’s cells are typically adept at processing the detritus of their normal functioning. Using specialized disposal systems known as the proteasome and lysosome, they can break down damaged proteins and worn-out parts, preventing the toxic build-up of waste.
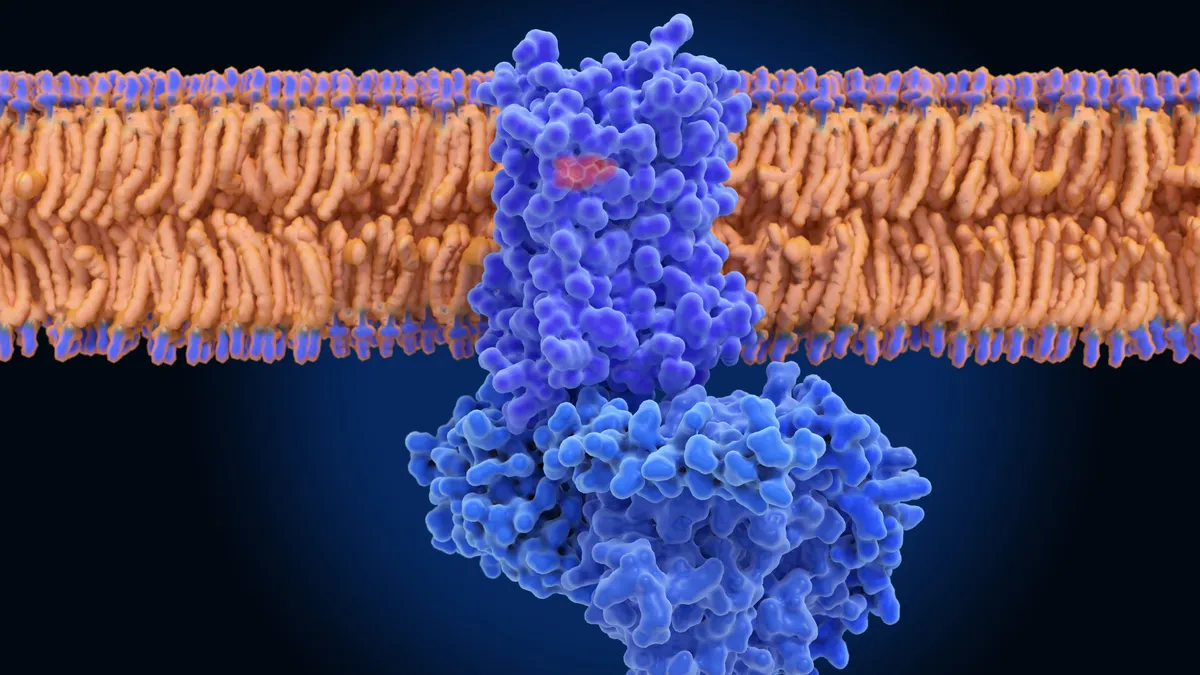
One of the main ways they do this is via a miniscule tag called ubiquitin. A ubiquitin tag marks cellular trash as such, spurring the cell to dispose of it.
But the cell doesn’t always recognize which proteins are harmful to it. Scientists have spent decades trying to figure out how to coax the process along and direct it toward proteins known to be associated with disease.
The result of their research is what’s now described as targeted protein degradation, which conceptually is a bit like ordering a junk hauling service for the cell. Specially designed small molecule drugs can bring together target proteins with an enzyme that tags them with ubiquitin, thereby marking them for destruction.
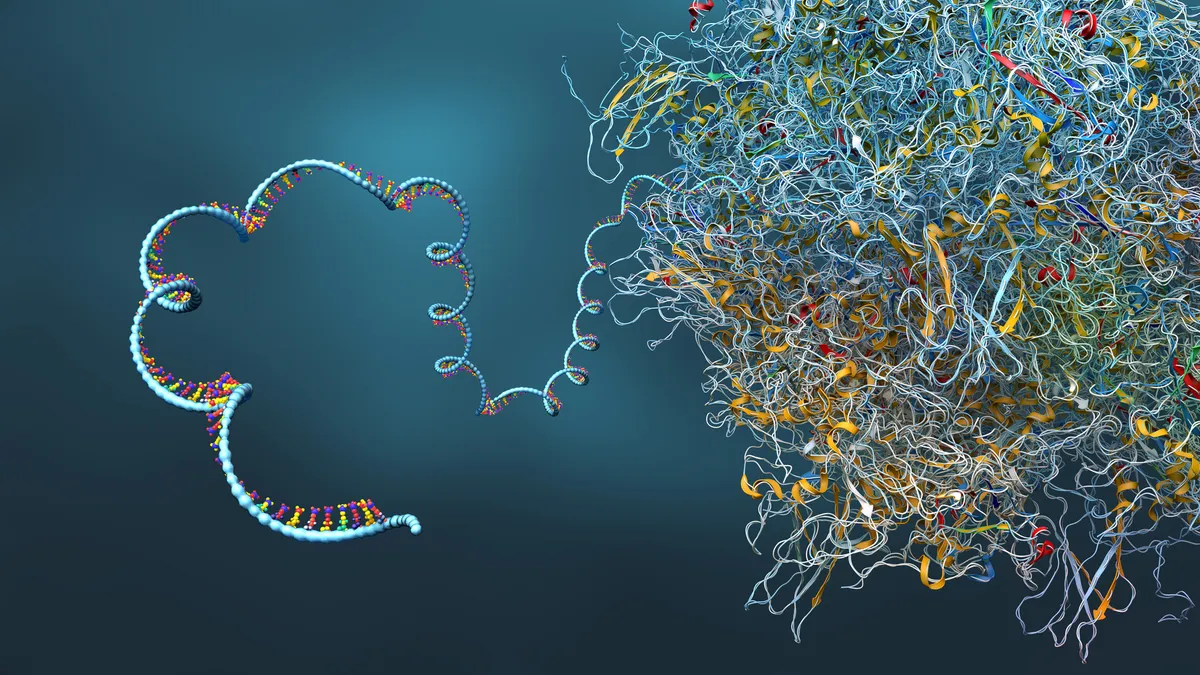
In their 2001 paper, Crews, Deshaies and others described how synthetic molecules could attach ubiquitins to unwanted cell parts. This approach drew attention as a way to go after proteins that typically can’t be bound by traditional drugs, which lock onto “pockets” amid the jumble of a protein’s amino acids. Later, in the 2010s, scientists realized that several blood cancer drugs made by Celgene worked via protein degradation.
"It was serendipitous as a discovery," said Nathanael Gray, a Stanford University professor who studies targeted protein degradation. The success of Celgene’s drugs, he added, “catalyzed the business and clinical interest” in the drugmaking approach.
Small molecule degraders generally consist of three parts: one component designed to bind to protein targets; a so-called E3 ligase recruiter, which attracts the enzyme responsible for tagging the problematic protein or cell part; and a linker.
“The beauty of PROTACs is that, for the first time, you could actually hijack the cell's natural ubiquitin-proteasome machinery and target specific targets,” said Cacace.
For years, researchers struggled to develop an effective method for directing the E3 ligase. But the discovery in the mid-2010s of some subtypes of ligands, and how they were expressed across cell types gave companies like Arvinas, C4 and Kymera better means to develop degrader drugs.
Cacace, of Arvinas, said those discoveries were “key pieces” that helped companies “bridge to greater tools” and led to oral drug-like molecules. "It really did give us this leap forward," Cacace said.
From there, the industry has invented several variations of the broader concept. Since Crews launched Arvinas in 2013, various biotechs have set out with their own spins on the idea, chasing different degrader pathways to the lysosome or proteasome.
Most focus on PROTACs or “molecular glues,” which are in development at companies such as Monte Rosa Therapeutics and Neomorph. They’re smaller than their PROTAC cousins, by not requiring a linker, but can be harder to design and optimize. Glues can be used, for instance, to introduce or restore communication between pathways that prompt cell death, which tumor cells have typically adapted themselves to avoid.
“You sort of create a Frankenstein situation,” Gray said, of molecular glues.
Molecular glues offer companies a means to tap into a broader concept called induced proximity, where the goal is similarly to draw two proteins together, but potentially for purposes other than degradation. Magnet Biomedicine, which recently struck a deal with Eli Lilly, aims to use molecular glues to spark cooperative protein-protein interactions.
And some, like Vicinitas Therapeutics, are developing deubiquitinase-targeting chimeras, or DUBTACs. While a PROTAC works by putting labels on harmful proteins that need to be trashed, DUBTACs remove those tags to save helpful proteins. The latter approach is useful if, for instance, researchers want to protect tumor-suppressing proteins.

What are the advantages of protein degraders?
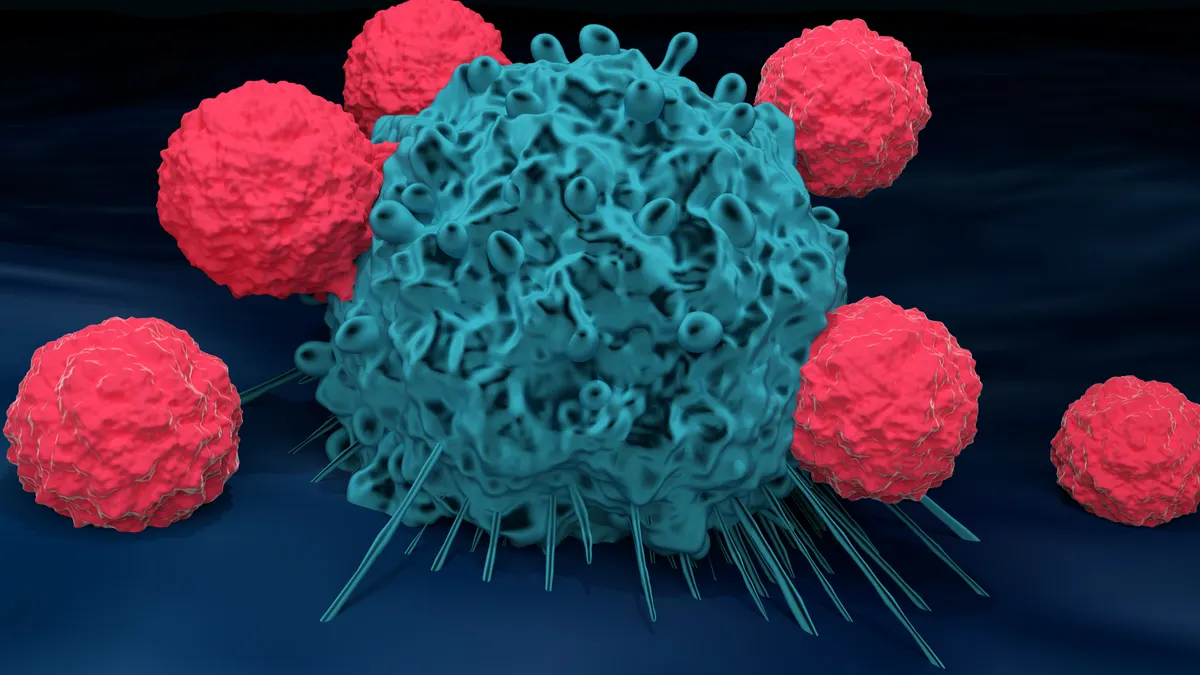
One of targeted protein degradation’s main draws is the path it offers to reach “undruggable” targets.
An estimated 85% of human proteins can’t be effectively targeted by typical small molecule drugs. And intracellular proteins, protected by the cell’s membrane, can’t be readily reached by biologic medicines like antibodies.
Small molecule degraders expand the universe of targets, as they don’t need to latch onto proteins in the ways that conventional drugs do.
Kymera’s oral degrader KT-621, which targets STAT6, is a good example. STAT6 is aimed at a transcription factor related to two cytokines, IL-4 and IL-13, that are important to immune cell function. Medicines hitting those receptors generate billions of dollars in annual sales for their makers. Dupixent, which blocks IL-4, alone brought in more than $4 billion in sales for Sanofi in the first quarter of 2025.
With KT-621, Kymera hopes to reach earlier in the process and better attack the underlying roots of disease. The idea of going in the cell with an oral drug has always been the holy grail for any disease, and especially in immunology, where these are chronic therapies,” Mainolfi said.
Protein degraders also hold potential to more efficiently knock out targets that already can be drugged. Arvinas’ vepdegestrant, for instance, works by tagging estrogen receptors for decay, reducing how much they are expressed in people with ER-positive, HER2-negative breast cancer.
Arvinas had hoped its drug would broadly outperform fulvestrant, an older type of drug known as a selective estrogen receptor degrader, or SERD. It positioned vepdegestrant as an alternative that doesn't require injections with fewer side effects. But mixed results in testing could cloud that particular drug’s future.
Andrew Hirsch, CEO of C4 Therapeutics, also notes how degraders could hold advantages because of the specificity they can achieve by co-opting ligases to recognize target proteins. With drugs that work by binding to their target — either reversibly or covalently — there are “still some off-target effects that you have,” he said.
Which companies are active in the field?
Of all the companies that have launched since the beginning of the last decade, the most advanced is Arvinas, which has with Pfizer filed an application for approval of vepdegestrant in people with ER-positive, HER2-negative breast cancer and mutations in the ESR1 gene.
Though it may not be used across a broader patient population, results from Arvinas and Pfizer’s trial of vepdegestrant offer some validation for degraders’ potential. The company is looking at another clinical prospect in B-cell lymphoma, as well as other programs in cancer and neurological disorders.
Following closely behind are Kymera and companies like Nurix Therapeutics. Kymera, which hopes to make oral drugs with biologic-like efficacy, released data for KT-621 in June, which showed treatment was well-tolerated in healthy volunteers. KT-621 completely degraded STAT6 in all participants who received multiple doses — "important validation for the target," according to Leerink Partners analyst Faisal Khurshid.
STAT6 is related to two popular drug targets, IL-4 and IL-13. Medicines hitting those receptors generate billions of dollars in annual sales for their makers; Dupixent alone brought in more than $4 billion in sales for Sanofi in the first quarter of 2025. “The idea of going in the cell with an oral drug has always been the holy grail for any disease, and especially in immunology, where these are chronic therapies,” Mainolfi said.
Also in the clinic are biotechs like Biohaven, which has a small molecule it’s developing to degrade IgG antibodies; Monte Rosa, which has three programs in Phase 1 testing for immune diseases and cancers, and C4, which is testing its treatment in patients with multiple myeloma and non-Hodgkin lymphoma.
Other targeted protein degradation companies are trying out new degrader technologies, among them Nurix Therapeutics and Orum Therapeutics. Both are developing treatments that draw on the idea of antibody-drug conjugates, but swap out the chemotherapy toxin for a protein degrader.
Pharma has struck up more than a dozen collaborations across the field. Roche has invested multiple times in molecular glue and degrader candidates, extending deals to C4, Monte Rosa Therapeutics and Orionis Biosciences.
Though those collaborations are “years away” from hitting the market, Roche sees “high potential” in pursuing those targets, said Boris Zaïtra, the head of corporate business development at Roche, in an interview earlier this year.
Orionis launched with a collaboration already in place with Novartis, which has partnered with Monte Rosa and Arvinas, too. Sanofi has struck up partnerships with both Nurix and Kymera.
Select companies working on protein degraders and molecular glues
| Name | Modality | Stage of development* | Notable partnerships, if applicable |
|---|---|---|---|
| Arvinas | PROTACs | Phase 3 | Pfizer |
| Kymera Therapeutics | PROTACs, molecular glues | Phase 1 | Sanofi, Gilead |
| C4 Therapeutics | PROTACs, molecular glues | Phase 1/2 | Roche, Biogen, Merck and Co., Merck KGaA |
| Nurix Therapeutics | PROTACs, degrader-antibody conjugates | Phase 1/2 | Gilead, Sanofi, Pfizer |
| Halda Therapeutics | RIPTACs | Phase 1/2 | |
| Monte Rosa Therapeutics | Molecular glues | Phase 1 | Roche, Novartis |
| Biohaven | MoDE / TRAP | Phase 1 | |
| Cullgen | PROTACs, degrader-antibody conjugates | Phase 1 | Astellas |
| EpiBiologics | EPITACs | Preclinical | |
| Orionis Biosciences | Molecular glues | Preclinical | Roche, Novartis |
| Magnet Biomedicine | Molecular glues** | Preclinical | Eli Lilly |
| Vicinitas Therapeutics | DUBTACs | Preclinical | |
| Parabilis Medicines | Helicons | Preclinical | |
| Lycia Therapeutics | LYTACs | Preclinical | Eli Lilly |
*Stage of development listed is specifically for those drugs that work by targeted protein degradation. **Magnet Biomedicine aims to induce cooperative protein-protein interactions, rather than degradation. Note: This table has been updated to correct the modality of protein degrader Biohaven is developing. SOURCE: Companies
What’s next for targeted protein degradation?
Arvinas and Pfizer, which presented a fuller picture of their vepdegestrant study at the American Society of Clinical Oncology’s annual meeting last month, filed an application for approval to the Food and Drug Administration on June 6.
If approved, vepdegestrant would be the first PROTAC drug cleared for commercial use. But hurdles remain. The two partners, despite filing for approval, have pared back two other planned trials of vepdegestrant and Arvinas cut one-third of its staff in May.
Kymera is proceeding with its Phase 1b trial testing KT-621 in patients with atopic dermatitis, and will launch Phase 2b studies in eczema and asthma later this year and early next. It's also advancing a drug candidate codenamed KT-485 for immune diseases with Sanofi, as well as a molecular glue candidate for cancer with Gilead.
Monte Rosa has two molecular glue prospects in early studies: MRT-6160, its collaboration with Novartis, is in testing with healthy volunteers, while MRT-2359, a wholly owned program, is being studied in people with lung and blood cancers. A third, MRT-8102, was cleared for human testing in June.
C4 has several prospects in early-stage testing for cancers.
Newer startups are pushing forward with different applications of the targeted protein degradation concept. EpiBiologics, for example, is developing targeted antibodies that go for extracellular proteins. Crews, in 2023, helped launch Halda Therapeutics, which is testing a spin on a concept called induced proximity by getting one protein to “smother” the other.
As always in biotech, there’s reason to be skeptical these efforts will all bear fruit. “Whenever you propose something new, smart people can tell you 50 reasons why it's not going to work, certainly, and usually at least one of those 50 reasons turns out to be true,” said Gray, the Stanford researcher.
But the “serendipitous” discovery of how degraders work more than two decades ago gave researchers hope to cling onto through their research’s ups and downs, he said. “There’s a real burning desire to show more progress.”
Jacob Bell contributed reporting.
Correction: This story has been updated to clarify the goal of research conducted by Magnet Biomedicines.